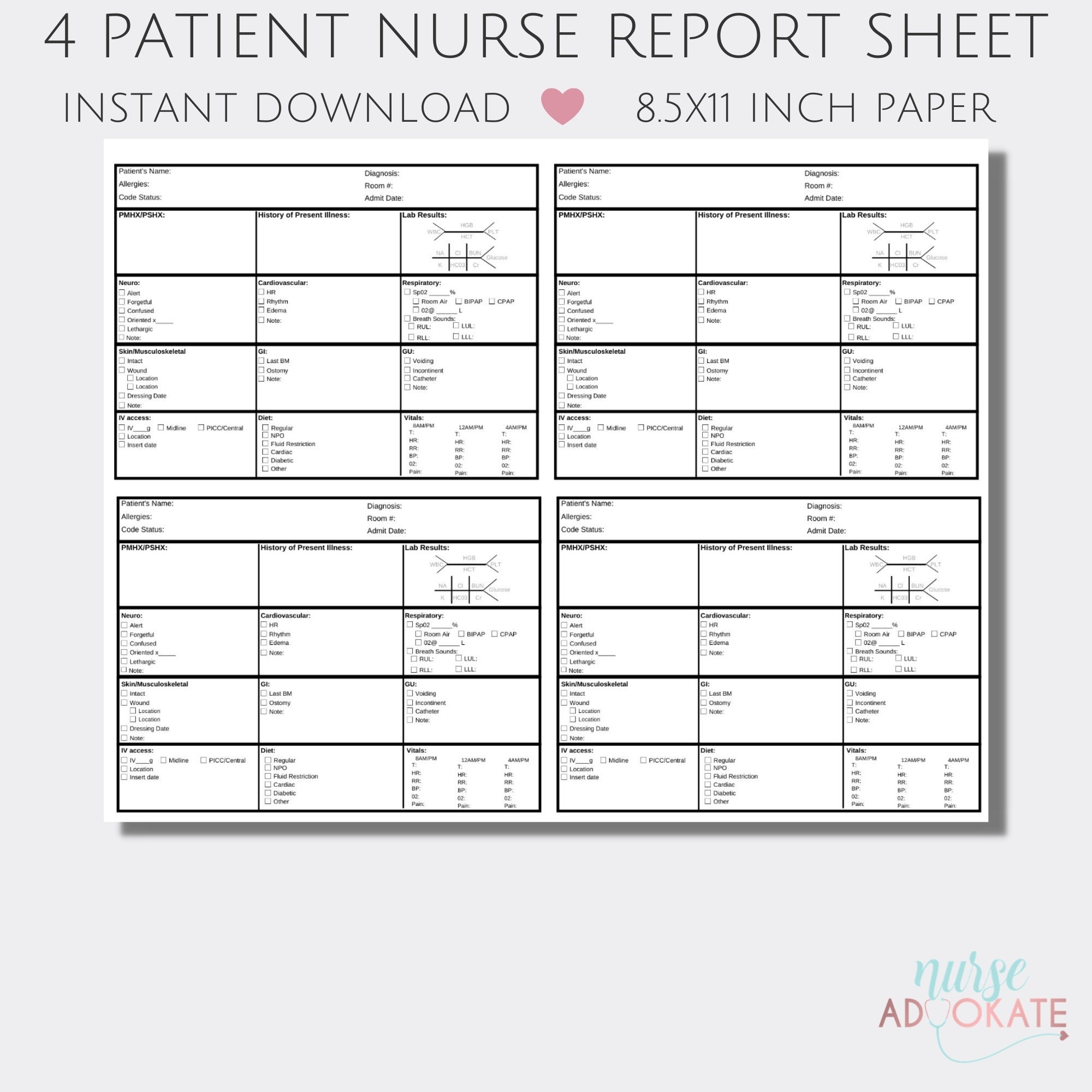
nursing report sheet b etsy 4 patient night shift report sheet nurses
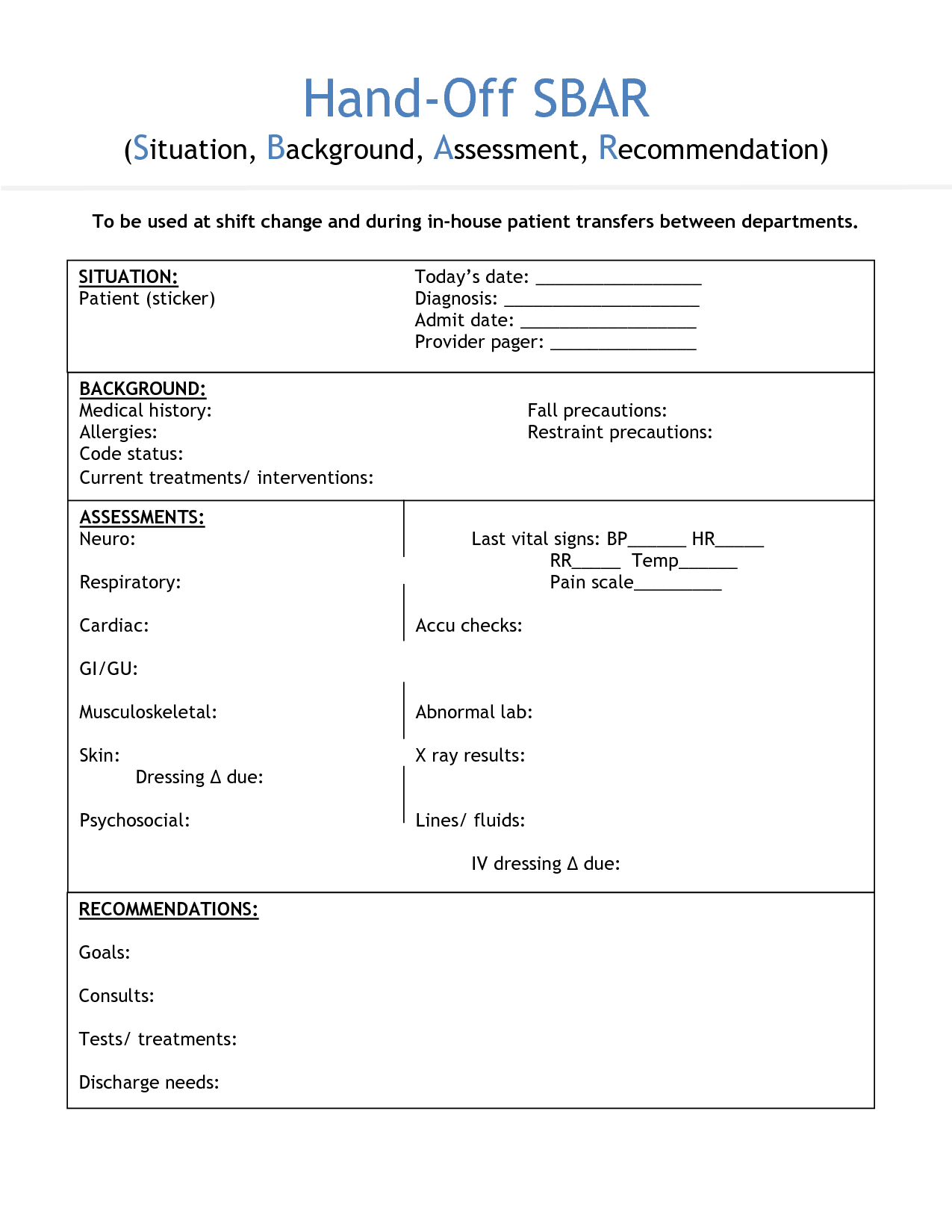
SBAR (Situation, Background, Assessment, Recommendation) is a verbal or written communication tool that helps provide essential, concise information, usually during crucial situations. In some cases, SBAR can even replace an executive summary in a formal report because it provides focused and concise information.
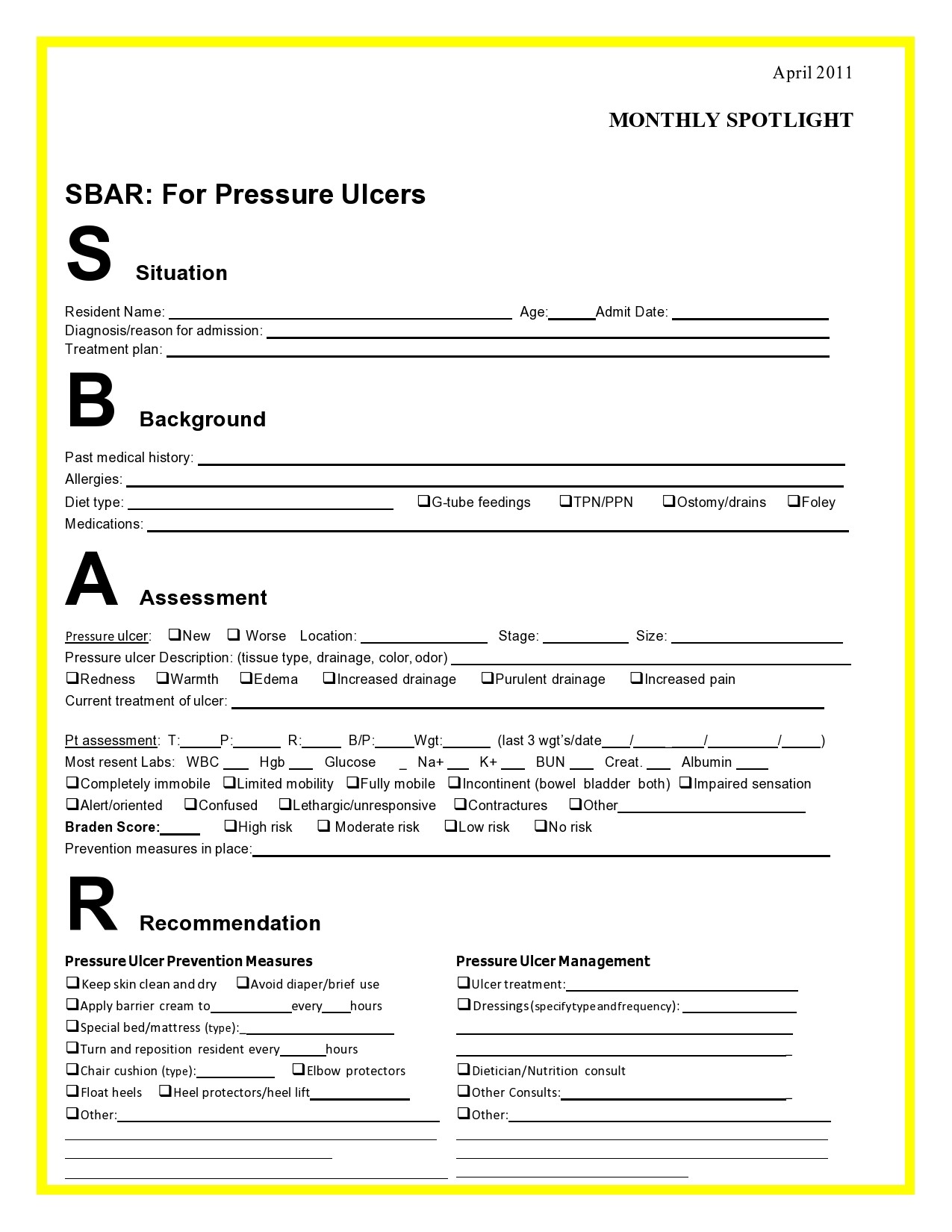
Sbar Report Template
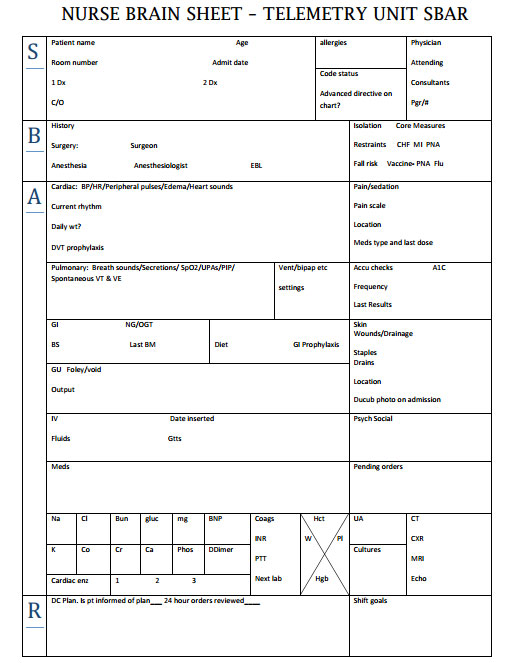
The SBAR (Situation, Background, Assessment, Recommendation) tool is used by all nursing fields within primary and secondary healthcare environments to aid patient safety ( NHS Improvement, 2018 ). Acts of communication through handovers, ward rounds, shift exchanges and team meetings are examples of when information is exchanged between nurses.
free sbar template for nurses Sbar Report Sheet Template Nurse report
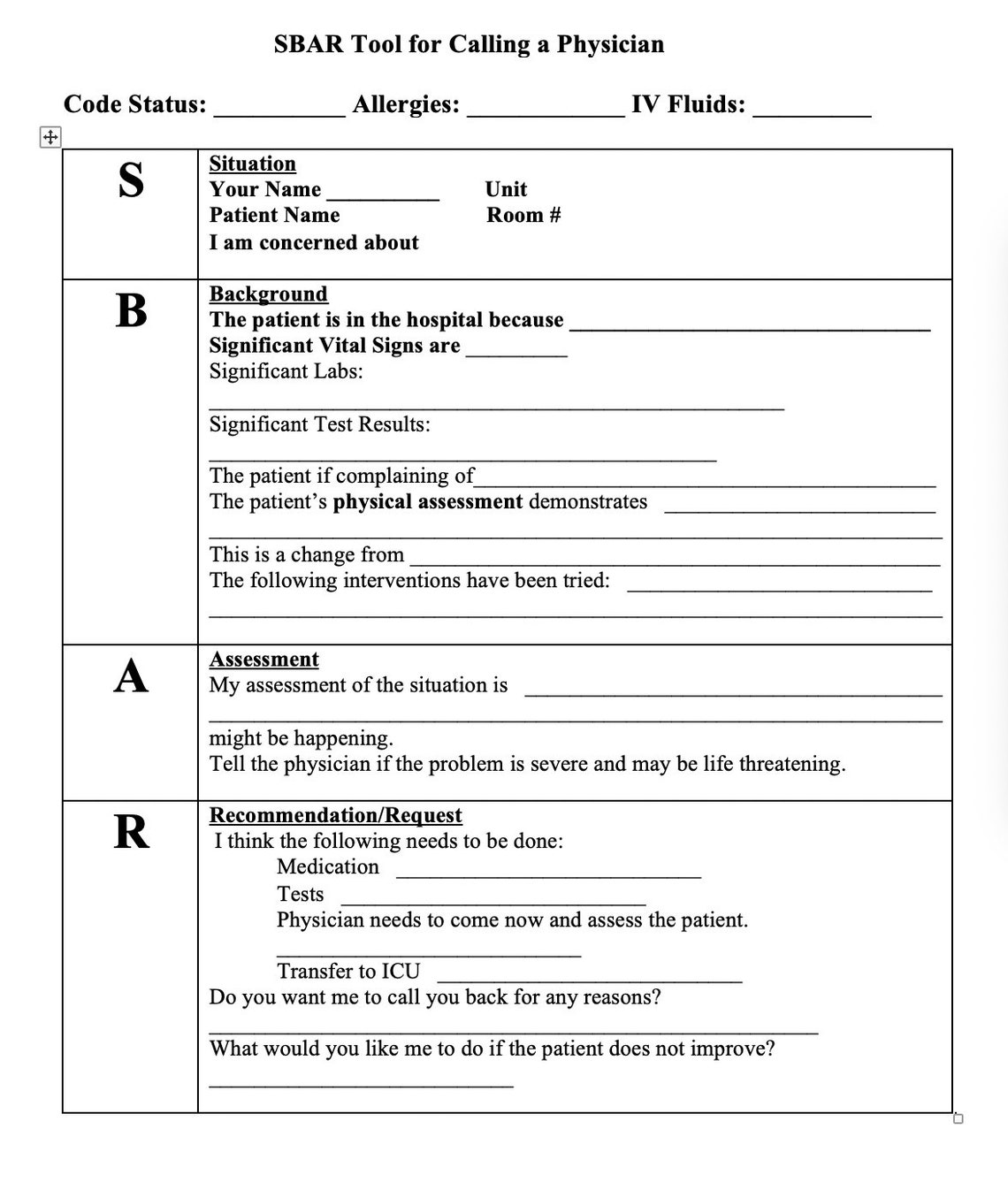
NHS England and NHS Improvement SBAR communication tool - situation, background, assessment, recommendation What is it? SBAR is an easy to use, structured form of communication that enables information to be transferred accurately between individuals.
Sbar Sheet FREE DOWNLOAD Freemium Templates
An SBAR report is a tool of communication between members of the healthcare team about a client's condition that follows the SBAR communication technique. SBAR stands for: S ituation B ackground A ssessment R ecommendation What is the purpose of the SBAR technique?

Printable Blank Sbar Template
What is SBAR? SBAR is a standard to communicate medical information. Simply, it improves accuracy and helps to correct dangerous errors. It Stands for: (Situation, Background, Assessment, Recommendation) The above four terms are the key facts. However, all should be conveyed properly.
Sbar Examples Nurse To Doctor One Checklist That You Should Keep In
An SBAR Report Template serves as a structured framework for facilitating clear and effective communication among healthcare professionals regarding a patient's condition, particularly in situations demanding prompt intervention.
Printable Nursing Handoff Report Template
7 Min Read Published April 26, 2023 What Is SBAR Used For in Nursing? What Does SBAR Stand For? How to Use SBAR for Communication SBAR Examples History of SBAR Key Takeaways SBAR is an easy-to-remember acronym that helps healthcare professionals communicate quickly, efficiently, and effectively.
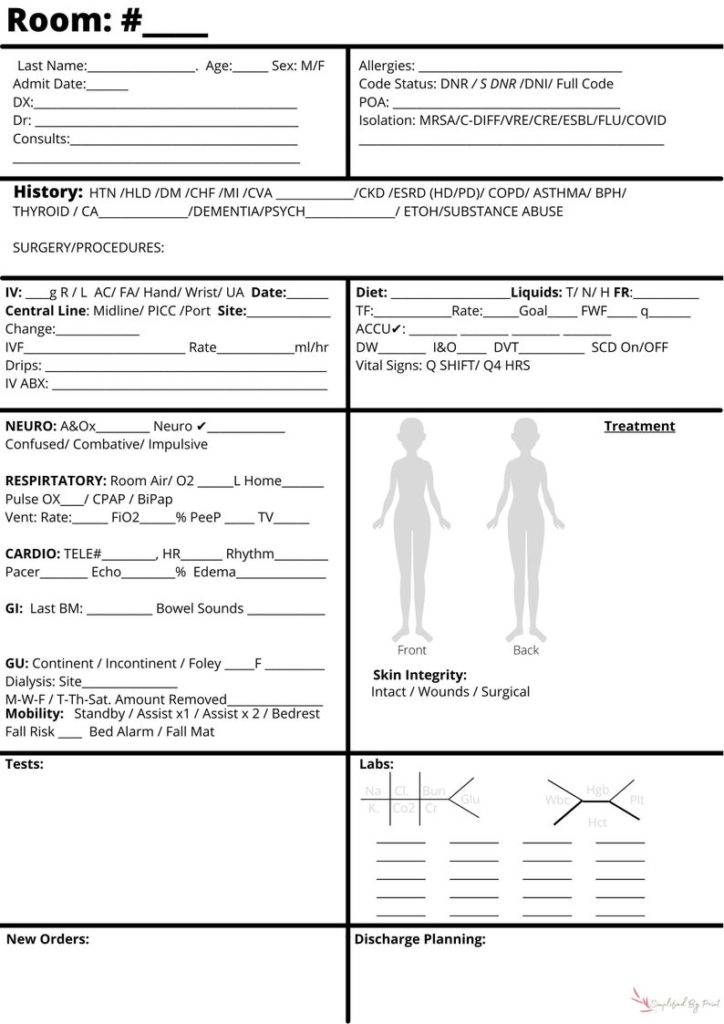
Nursing SBAR Bedside Report Sheet Simplified by Print
Download this free SBAR template to efficiently document the Situation, Background, Assessment, and Recommendation about a particular patient or case. Using this template, be able to completely provide information to help ensure continuity of patient care by doing the following:

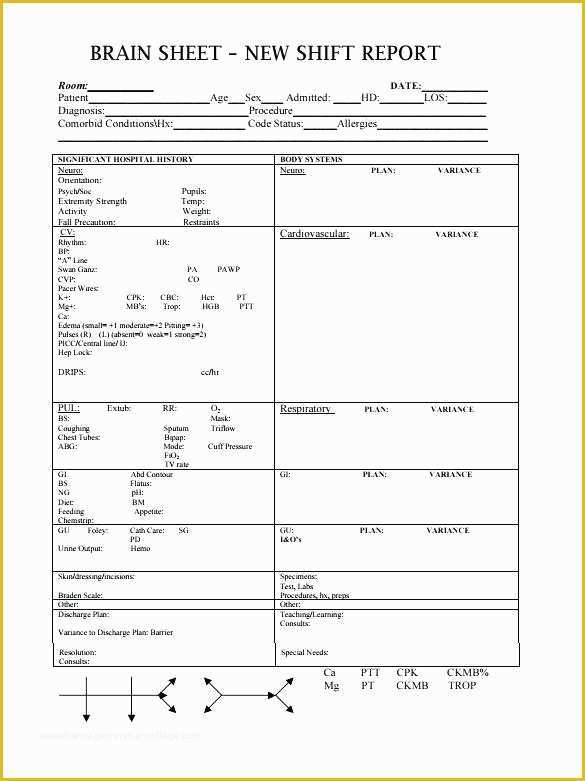
197 best Nursing forms & templates images on Pinterest Nursing
SBAR stands for Situation, Background, Assessment, and Recommendation—an effective framework for conveying critical information between healthcare professionals. Our customizable and printable templates provide a structured approach to communicate patient conditions, vital signs, medical history, and recommended actions.

Sbar Nursing Shift Report Form On Sbar Nursing Worksheet Med Surg
13 Blank SBAR Templates (Word, PDF) SBAR is an acronym for Situation, Background, Assessment, Recommendation. It is a technique used to facilitate appropriate and prompt communication. An SBAR template will provide you and other clinicians with an unambiguous and specific way to communicate vital information to other medical professionals.

Free Printable Nursing Handoff Report Template Printable Form
The SBAR (Situation-Background-Assessment-Recommendation) technique provides a framework for communication between members of the health care team about a patient's condition. SBAR is an easy-to-remember, concrete mechanism useful for framing any conversation, especially critical ones, requiring a clinician's immediate attention and action.

Free download! This is a fullsize SBAR nursing brain report sheet. 1
Free downloadable tools to support your work to improve health care quality and safety at every stage — from establishing a project plan and an improvement aim, to understanding a process, to identifying root causes or drivers, to testing changes using PDSA cycles, to implementing and spreading successful improvements, and more. Featured Tools

Nurses Report Sheet Nurse Report Sheet Nurse Brain Sheet Sbar Images
Safer Care SBAR Situation • Background • Assessment • Recommendation Implementation and Training Guide
Free Printable Sbar Template Of Sbar Hand F Report Sheet Nursing
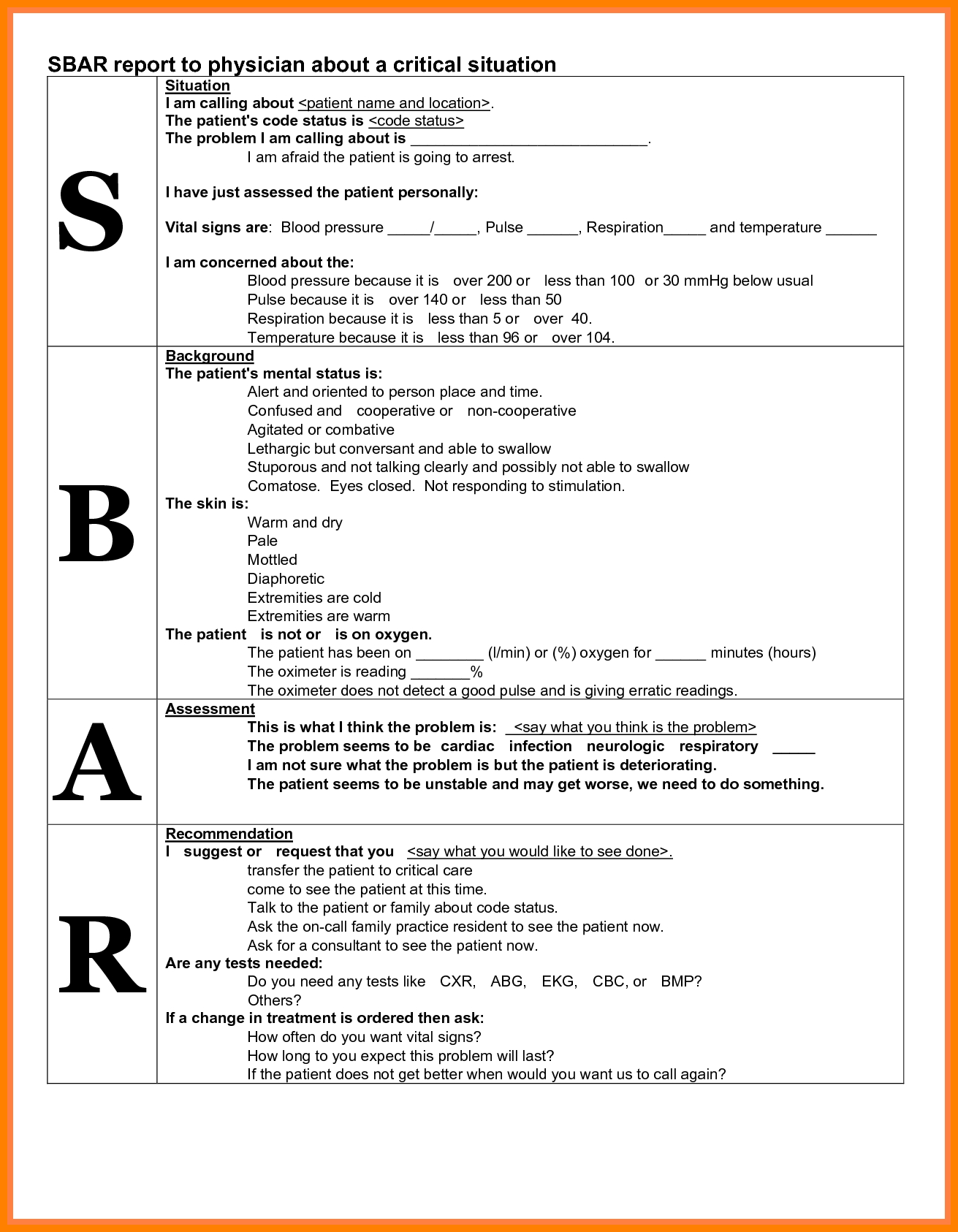
SBAR Worksheet ("SBAR report to physician about a critical situation"): A worksheet/script that a provider can use to organize information in preparation for communicating with a physician about a critically ill patient

Sbar Template Word Business Design Layout Templates
SBAR is an easy to remember mechanism that you can use to frame conversations, especially critical ones, requiring a clinician's immediate attention and action. It enables you to clarify what information should be communicated between members of the team, and how. It can also help you to develop teamwork and foster a culture of patient safety.

Paper & Party Supplies Stationery Nurse Report Sheet SBar & Brain
SBAR Worksheet: A worksheet/script that a provider can use to organize information in preparation for communicating with a physician about a critically ill patient (includes both an example and a blank SBAR Worksheet template) Both the worksheet and the guidelines use the physician team member as the example; however, they can be adapted for use.